Enhancing Code Blue Workflow for Improved Survival Rates

Code blue workflow: Introduction
In critical healthcare scenarios, swift response is the linchpin to saving lives. Enter code blue workflows – a set of protocols that guide healthcare teams in high-stress scenarios. When a patient’s life is at stake due to cardiac arrest, respiratory failures, or other life-threatening conditions, these workflows ensure a rapid, synchronized response.
While much has been written about code blue workflows, there’s not a lot out there that describes how to improve a code blue process and minimize the time it takes to respond to a patient. In this blog, we discuss how code blue workflows can be optimized with the ultimate goal of improving the survival and discharge rates of patients.
Challenges that permeate healthcare organizations
Despite the significant strides in healthcare, it’s astonishing to find that several life-critical workflows are still hindered by inefficiencies. Hospitals continue to grapple with siloed systems that, while beneficial in isolation, contribute to fragmented communication within the broader healthcare ecosystem. These disparate health systems hold significant information about patient’s health, but due to their lack of synchronous communication with one another, they fail to compound their benefits.
As a result of these inherent inefficiencies, healthcare teams find it challenging to deliver optimal care, hindered by incomplete information for informed decision-making, which unfortunately takes a toll on patient health.
A study conducted by researchers at the University of Maryland Medical Center in Baltimore highlighted a remarkable statistic: when care providers were promptly notified of a code blue situation through their secure smartphone clinical communication app, the patient survival rates went up by an average of 8%, from 17% to 25%. Building upon this research and drawing from our extensive sector expertise, we present a clinical communication workflow with significant potential to enhance code blue workflow responses.
Try OnPage for FREE! Request an enterprise free trial.
Traditional Code Blue Workflows
Before diving into the optimization of code blue workflows, let’s examine a typical code blue workflow. It’s worth mentioning that every hospital may have its own unique code blue protocols; while some hospitals may closely resemble the procedures discussed in this blog, others might exhibit slight variations.
A typical code blue workflow initiates when a clinician contacts the hospital operator via phone to report a code blue incident. In certain hospitals, designated on-call hospitalists may handle this call. Alternatively, some organizations may require all staff members near the incident’s location to convene and contribute their expertise. Larger hospitals may offer dedicated teams specialized in resuscitating patients in such scenarios.
Subsequent to receiving a report, the operator is responsible for mobilizing the team, beginning with the announcement of “Code Blue” via the overhead PA (public address) system. This announcement might incorporate warning sounds and furnish information about the incident’s location, including details about the floor/level number and room number.
Upon receiving this alert, the designated teams promptly proceed to the location to address the immediate incident.
While assembling teams is paramount, it’s equally crucial to ensure that each member comprehends their assigned role upon being corralled. Those entrusted with tasks such as administering cardiopulmonary resuscitation (CPR) or using the defibrillator must know who they are.
There must be a designated member who is responsible for intercepting the family and taking them to a central area conference room for updates and counseling.
Here, you will witness Dr. Siobhan Deshauer, a popular YouTuber in the healthcare community, as she recounts a Code Blue emergency situation on her YouTube channel, ViolinMD. You will observe how an ordinary day quickly turns into an adrenaline-pumping roller coaster ride. You’ll observe how she and her team intervene when called to respond to a code blue page, swiftly moving a patient whose heart rate was declining into a monitored setting.
Here’s an example where you can hear a code blue page being broadcast on an overhead PA system.
Try OnPage for FREE! Request an enterprise free trial.
Crucial Seconds, Improved Survival with New Workflows
Moreover, the overhead paging system lacks the capability to provide comprehensive information about the patient’s condition. This limitation is intentional as it aims to prevent undue panic among neighboring patients and visiting family members. However, this dearth of contextual information at the disposal of the appropriate team exacerbates the challenge of gathering and promptly initiating life-saving interventions.
When seconds hold significant weight, healthcare professionals require an efficient means to swiftly communicate a patient’s situation while accurately mobilizing the appropriate team members. Moribund methods no longer serve any utility; instead, they hinder the process.
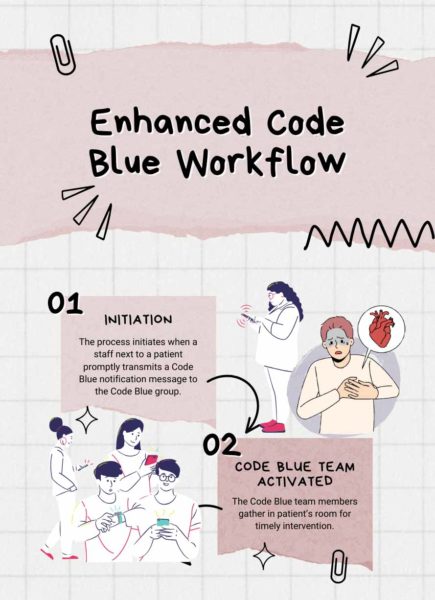
Let’s examine a workflow that addresses these challenges and enhances the response time from the moment an alert is triggered to the swift engagement of the Code Blue team.
The new workflow that we propose commences with the staff stationed next to the patient promptly transmitting a Code Blue notification message to the designated Code Blue contact group using just a few keystrokes. This pre-established Code Blue contact group would generally encompass a roster of experts, including on-call cardiologists, emergency medicine physicians, intensivists, anesthesiologists, critical care nurses, respiratory therapists, chaplains/social workers, and hospital coordinators.
Teams may find it beneficial to structure their Code Blue group in a manner that features specialized on-call subsets, each dedicated to a specific functional role. By bypassing intermediary steps described in the conventional approach, the staff member situated by the patient’s side can instantaneously activate the Code Blue team, facilitating an immediate response and the prompt administration of necessary interventions.
Clearly, enhancing emergency communication workflows holds the potential to expedite critical patient responses, arming healthcare teams with essential contextual knowledge about the patient’s health. This equips them to deliver immediate care the moment they arrive at the scene. In situations where time is of the essence, even a minute of earlier intervention can move the needle between life and death. As such, this innovative communication workflow has the power to offer patients suffering from cardiac arrest improved chances at a better life, potentially transforming their outcomes significantly.
Conclusion
In conclusion, optimizing Code Blue workflows is pivotal for boosting survival rates and patient discharges in critical healthcare scenarios. By streamlining processes and leveraging technology, swift responses can be achieved, ensuring timely interventions.
Traditional workflows, although well-intentioned, often suffer from inefficiencies that can lead to delays. Embracing innovative approaches, like our proposed workflow, empowers healthcare teams to act swiftly and effectively in life-threatening situations, ultimately saving more lives.