Hospital Discharge Best Practices
Best Practices for Hospital Discharge Processes

Establishing an effective hospital discharge process is a crucial part of a patient’s stay and can significantly impact the success of their recovery. Patients, families, and subsequent care providers require a detailed education on continued treatment, aftercare processes, and required medications, to avoid any complications that may surface during recovery.
The continued care that successful patient discharge offers, can also impact readmission rates. Many hospital readmissions can be avoided by providing more thorough discharge preparation. There are often many care providers involved in a single patient’s medical journey, as well as complex aftercare requirements that necessitate a structured discharge process that will ultimately reduce readmission rates.
In this blog, we provide an in-depth outline for hospital discharge processes along with best practices, so that hospitals can reduce complications for patients after their stay.
Outlining an Effective Hospital Discharge Process
Healthcare teams must develop an extensive patient discharge process that details all the necessary steps they must take. Ultimately, this will help teams to effectively eliminate the possibility of overlooking steps in the process and ensure the successful discharge of every patient.
To help your team establish a hospital discharge process, here is a outline that can guide them in the process:
- Prepare for discharge
Before patients are ready to be discharged, care teams must make the proper preparations. It is crucial to carefully assess their patient’s conditions to verify their suitability for discharge. Additionally, care teams are required to review all of the aftercare procedures and necessary medications to ensure that the plan is up-to-date. By performing these reviews, patients will be equipped with an effective aftercare plan customized to their specific needs.
- Educate the patient and their family
To avoid any confusion about medical conditions or aftercare plans, care providers need to provide patients with clear information to ensure their understanding. Patients and their family should be encouraged to ask any questions and raise any concerns they have about recovery as well, so that they understand their medical condition to the fullest extent facilitating a successful recovery.
- Manage necessary patient medications
Before discharging a patient, physicians must double-check the prescription, dosage and administration requirements on a patient’s necessary medications to avoid potential complications. And, patients must be given detailed documentation, so that they can effectively self-administer the medications without risking overdose.
- Coordinate all of the required arrangements
Some critical patients are transferred to care facilities that will provide ongoing care through their recovery. It is crucial that healthcare teams coordinate these arrangements accordingly. This could include equipping patients with the required medical supplies or making sure that they have sufficient transportation to their next location.
- Facilitate a home assessment
If a patient with a severe condition is headed home post-discharge, it is important that a home assessment takes place for a seamless transition. Care providers must evaluate the patient’s environment, identifying and making any necessary modifications that will improve the comfort and well-being of the patient during recovery.
- Provide detailed documentation
Patients may have a difficult time retaining all of the essential information regarding their recovery, so they must be equipped with detailed documentation that outlines the aftercare processes, home remedies, dietary restrictions, medication dosages, and administration requirements that can be taken home for review.
- Schedule follow-up appointments
Patients should be scheduled for follow-up appointments prior to their discharge. This ensures that patients receive timely follow-up care that does not get delayed by the care provider’s busy schedule. Follow-up appointments are crucial for identifying any medical complications that patients may have missed. Additionally, patients should be equipped with remote access to their care teams, so in the event of a complication they can promptly contact their doctor, and proceed with the recommended solution.
- Hand-off all information to the next care provider
Doctors must facilitate effective hand-off with subsequent care providers to guarantee that all of the patient’s requirements are successfully exchanged between providers. This includes developing strong clinical communication and collaboration plans that facilitate seamless communication.
- Seek feedback from the patient and their family
After discharging a patient, care providers should seek feedback from them to see where they could make adjustments to their procedures. By doing this, care providers can facilitate continuous improvements allowing them to consistently deliver quality care.
Try OnPage for FREE! Request an enterprise free trial.
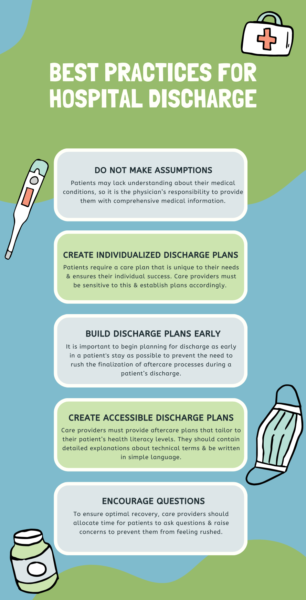
Best practices for hospital discharge
- Do not make assumptions
Oftentimes, patients lack understanding about their medical conditions, so it is the physician’s responsibility to provide them with comprehensive medical information. It is better for a physician to be excessively communicative than to place the burden on the patients to be aware, potentially causing them to miss vital aftercare steps.
- Create individualized discharge plans
Every patient has different needs, capabilities, and home lives that can impact their ability to successfully incorporate an aftercare plan into their daily lives. Care providers must be sensitive to this and develop individualized care plans for every patient.
- Build discharge plans early
It is important to begin planning for discharge as early in a patient’s stay as possible to prevent the need to rush the finalization of aftercare processes during a patient’s discharge.
- Write discharge plans that tailor to patient’s health literacy
Due to varying comprehension levels, care providers must provide aftercare plans that are tailored to the patient’s health literacy levels. They should use simple language wherever possible and have detailed explanations about technical terms when a patient is unaware of the term.
- Encourage patients to ask questions
When patients are being discharged, they can often feel rushed, causing them to keep their questions and concerns to themselves. To ensure optimal recovery, care providers should allocate time for patients to ask questions and raise concerns.
OnPage as a Solution
OnPage is an innovative clinical communication and collaboration tool that encourages healthcare providers to facilitate clear and accurate information exchanges ensuring successful patient discharge.
Some of OnPage’s features that can enhance the hospital discharge process are:
- HIPAA-Compliant Text Messaging
OnPage’s clinical communication and collaboration system is HIPAA compliant, allowing care providers to deliver contextual messages containing PHI that would otherwise be limited with unencrypted technologies.
- Two-Way Communication Capabilities
With two-way messaging capabilities, care teams can increase collaboration, thus improving the quality of care by encouraging knowledge sharing and follow-up questions between care providers working with the same patient. Two-way communication also facilitates patient handoffs during discharge, as care providers can seamlessly exchange critical information and ensure a smoother transition for the patient.
- Audit Trails
Legacy pagers often lose messages due to limited ranges and connectivity issues, but that is not a problem with OnPage. Because in the unlikely event that an OnPage alert does not go through immediately the sender can view the message’s status complete with SENT, DELIVERED, and READ indications.
- Live Call Routing
Rehospitalization can be preemptively avoided by giving patients access to care teams outside of the healthcare setting. OnPage offers dedicated lines with live call routing that can facilitate instant access to care teams. With live call routing, patients gain an expedited channel for emergency communication with their clinicians.